And doctors say it can take weeks for insurers to approve or deny certain treatments or tests. If the answer is no, the doctor who wishes to appeal must start the lengthy process again.
Doctors also say it’s exasperating to have to continually seek prior authorization for routinely approved procedures. They believe that doctors who have already received the green light for treatments or tests should be able to bypass this tedious process.
Dr. Debra Pattoncologist and breast cancer specialist in Austin, Texas, and medical director of public policy for the US Oncology Network, has testified before Congress on the issues facing cancer patients.
“There have to be responsible ways to use prior authorization,” Pratt said in an interview. “This has gotten completely out of control. I think patients are on a journey and prior authorization is like obstacles in the way that they may not be able to clear.
Texas has been at the forefront in combating delays and denials associated with prior authorizations. The state has passed legislation in 2021, known as the Gold Card Act, which exempted doctors from going through the authorization process if private insurers had approved their procedure submissions at least 90% of the time.
Last year, Texas passed a law exempting patients with autoimmune diseases from requiring prior authorization for their procedures. Dr. Ezequiel Silva, an interventional radiologist in San Antonio and chair of the Texas Medical Association Council on Legislation, said patients with cancer and other chronic illnesses should also have prior authorization exemptions.
“There are a lot of patients with chronic illnesses,” Silva said. “If we could find a way to exempt them from the prior authorization process, the gains for them could be monumental. »
New Medicare Screening Denials
Private insurance companies are not the only ones increasing the number of refusals of cancer care and screening. This year, women at risk for breast cancer began receiving reimbursement denials from Medicare for identical ultrasound exams approved by Medicare in 2023, according to patient documents.
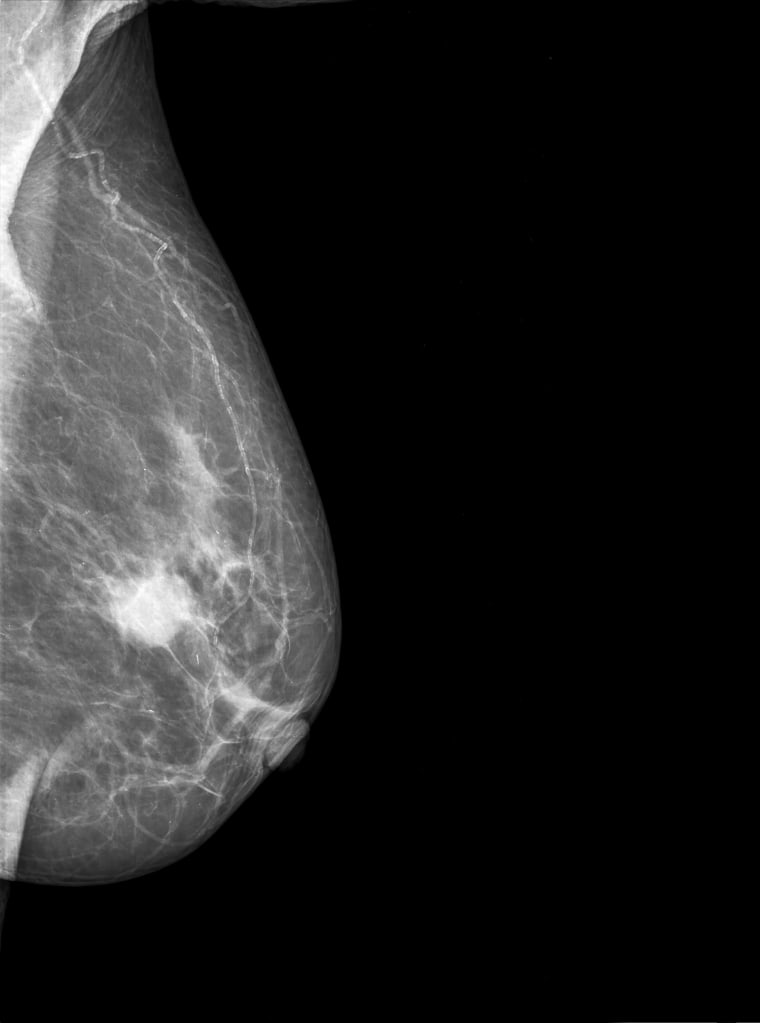
Ultrasound screenings identify cancers that may be missed in mammograms, radiologists say. And they’re imperative for women with dense breast tissue, a condition that affects nearly half of women over 40, according to the Institute. National Institutes of Health.
Dr Madhavi Raghu, a radiation oncologist in Connecticutprovided NBC News with several redacted patient records showing Medicare was denying reimbursements in 2024 for breast ultrasound screenings that it had reimbursed in 2023. The records represent a small sample of the denials, she said.
Raghu said this change is particularly surprising because it occurs in the same year as the start of the Food and Drug Administration. demanding mammography providers to inform patients with dense breast tissue that they may need additional cancer screenings. These additional exams include MRIs and ultrasounds for which Medicare denies coverage.
“It’s unfair to tell a patient that you have an increased risk of developing cancer and we have another test to detect it, but you will have to pay for it,” Raghu said. “It upsets me to see patients presenting with stage 3 breast cancer because they have not had the opportunity to be screened beforehand.”
NBC asked a Centers for Medicare and Medicaid Services spokeswoman about this reimbursement change and provided her with documents showing 2023 acceptances and 2024 denials. She said CMS’ coverage policy does not had not changed.
“The ultrasounds or MRIs you are referring to are covered by Medicare when provided as a diagnostic test,” the spokesperson said. “If the scans were provided as a screening test, then Medicare is not able to cover them by law.”
Raghu pointed out that there is only one reimbursement code for a breast ultrasound, whether it is offered as a screening or diagnostic test. As a result, Medicare’s systematic denials this year appear to place all breast ultrasounds in the uncovered category.

Sumrall, the North Carolina neuro-oncologist, said she, too, has seen Medicare deny many other requests for breast ultrasounds this year and has heard the same thing from other doctors.
“No one can understand how Medicare made this decision,” Sumrall said. And as private insurers shift to Medicare reimbursement for their policies, “that means more private insurers will follow what Medicare does.”
The Department of Health and Human Services did not respond to a request for comment regarding the reimbursement change.
Potential life sentence in every denial
Hsu’s difficulties with insurers began in 2015, at an otherwise happy time in his life. She was diagnosed with breast cancer right after her engagement to her husband. Hsu, a New York resident, underwent surgery and chemotherapy, but the cancer spread to her spine and sternum in 2018.
In response, she began aggressive immunotherapy treatments with quarterly PET scans to monitor her metastatic breast cancer. Hsu continued to work and gave birth to her daughter, now 4 years old.


