Esophageal adenocarcinoma (EAC), one of the two main forms of esophagus cancer, is the most deadly sixth cancer in the world for which there is no effective targeted targeted therapy. Patients must rely on chemotherapy as a standard of care, which is launched before surgical interventions as so-called “neoadjuvant” (NACT) chemotherapy in the hope of shrinking or controlling tumors. However, most patients become resistant to certain NACTs, leading to poor results.
Given the total lack of therapeutic alternatives, respondents and non-respiants, continue to receive one of the chemotherapy available without knowing if it will work. Even among responders, choice chemotherapy may not completely prevent their tumors from progressing and metastasizing, and it can have toxic side effects on the body. The availability of a personalized precision oncology model and specific to the patient who can precision predict a patient’s response to the different NACTs in a timely time is a critical non -satisfied need.
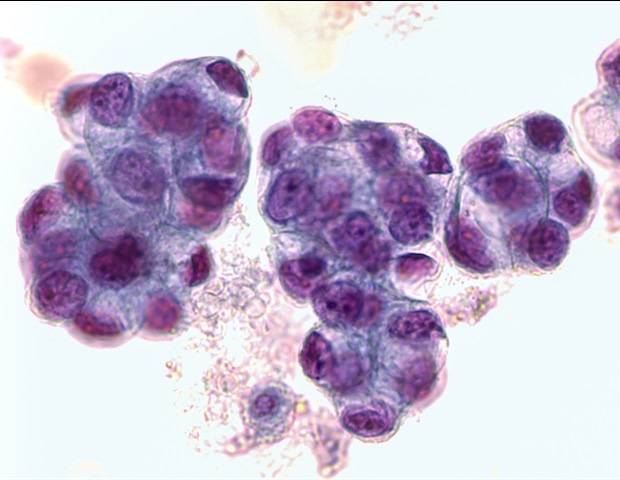
The researchers had cultivated so-called “organoids” of biopsied EAC cells, which are 3D esophageal mini-organizations formed with stem cells specific to tissues which have critical characteristics of the esophageal epithelial lining. However, these lack important components of the specific tumor microenvironnement of a patient (TME), such as Stromaux fibroblasts and collagen fibers, and therefore, they do not show the same responses to NACT as real tumors.
Now, a research collaboration led by Donald Ingber, MD, PH.D., founding director of the Wyss Institute for Biological Engineering at Harvard University and Lorenzo Ferri, MD, who heads the Thoracic and Upper Gastrotine Surgery Division of the McGill University Health Center in Montreal, has progressed a personalized medicine solution with the potential to improve Chemotherapy for EAC patients for EAC patients.
Researchers have exploited the microfluidal culture technology of the Wyss Institute human organ chip and used it to co-culture the EAC organs alongside stromal cells isolated from the same biopsies as the MCGill team obtained from patients with CAC in a clinical cohort study to create models of cancer with TME inclusion of TME specific to the patient. By summarizing part of the complexity inherent in TME in vitroThe team was able to predict the tumor responses of patients at the standard NACT much more precisely than less static and less complex 3D organoid models. Since the approach can produce results within 12 days of starting the model, it allows rapid stratification of CAE patients in respondents and non-response, and the study of non-standard NACTs depending on different chemotherapy agents for resistant patients within a clinically useful time. The results are reported in Journal of Translational Medicine.
This patient -centered approach is strongly based on our previous successes using human organ fleas technology to summarize thetone of each cancer patient outside of his body so that we can identify the combination of drugs that will best work for this very patient. This new way of approaching personalized medicine could be implemented in clinical centers by focusing on patient care with many different types of cancer, such as that led by our employees with patients with esophagus cancer. Perhaps just as important, it can also be used as a preclinical trial bed to innovate in the development of therapies targeted by tumor or in stroma for cancer patients and allow the discovery of biomarkers who could be used to monitor and optimize the effects of drugs in these patients. “”
Donald Ingber, MD, PH.D., founding director of the Wyss Institute for Biological Inspired Engineering at Harvard University
Ingber is also the Judah Folkman professor of vascular biology at the Harvard Medical School and at the Boston children’s hospital and Hansjörg Wyss Biological Inspiration Engineering At the Harvard John A. Paulson School of Engineering and Applied Sciences.
Modeling of esophageal pathologies
The Ingber and Ferri teams have already started to collaborate in 2023 in a previous study in which they modeled the Barrett esophagus in a microfluidic organ chip with vital support by the National Institutes of Health (NIH) and Cancer Research UK. The Barrett esophagus can be a clever precursor of the EAC, which is considered to be the result of a series of pathological changes that the epithelial lining of the lower esophagus is in progress. These begin with inflammationwhich is most often induced by acid refluxcontinue via The transformation of the esophageal fabric into the hyper-prolifier stomach and the intestinal type tissue (Barrett esophagus), to finally lead to the conversion of these abnormal cells very proliferating into cancer cells. Above all, these malignant changes are not only driven by molecular and cellular processes in the epithelial mucosa of the esophagus, but also in its underlying “stroma”, which is composed of fibroblast cells which communicate with cancer cells by a constant exchange of molecules, and it also contains immune cells and blood vestiges.
“While in our previous works, we have faithfully summarized the previous stages of the pathological process potentially leading to the EAC, namely the esophagus of Barrett, in our new study, we were quickly launched in its cancerous result,” said the second author Elee SHIMSHONI, PH.D., who was a postdoctoral scholarship holder in the two studies. “It is only by reconstituting the key components of TME and by imitating some of its liquid flow rates, which are normally supplied by cells surrounding liquid (interstitial liquid) and in support of blood vessels, we were able to obtain exposure to physiologically relevant drugs, and to predict precisely the specific responses to the patient.
Patients with cancer and back chips
The team designed their EAC-ITEMP chip by first generating personalized EAC organs from biopsies that they obtained in endoscopically from patients who were recently diagnosed with EAC but who had not yet been treated. First author Sanjima Pal, Ph.D. and other members of the Ferri team at the McGill University Health Care where Ferri treats patients with esophagus cancer, had mastered the ability to create esophageal organs with a patient with strong coherence. Then, the team withdrew the organoids from the culture box, broke them in their constituent cells, cultivated the cells in one of the two channels parallel to the parallel of a microfluidic chip the size of a memory stick. And added fibroblasts associated with tumors of the same patients to the other channel to form an adjacent tumor stroma. The two channels are separated by a porous membrane, which allows cancer and Stromal tissues to freely exchange molecules as they would in a real tumor. Finally, the researchers have increased a cocktail of triplet chemotherapy based on doctaxel in nutritious fluids circulating through the Stromal canal, using the concentrations of medication and exposure times which reproduce a cycle of chemotherapy in patients with PAE.
For a cohort of eight patients, all EAC chips predicted their answers to the NACT in the 12 days. In four of the chips, chemotherapy has killed the EAC cells, while in the other four tokens, the EAC cells survived chemotherapy. These results were perfectly correlated with patient responses to the same chemotherapy and their survival rates after surgical resection of EAC tumors.
The other authors of the study were Salvador Flores Torres, Mingyang Kong, Kulsum Tai, Veena Sangwan, Nicholas Bertos, Swneke Donovan Bailey and Julie Bérubé. It was funded by a Stromal reprogramming subsidy of the research of cancer of cancer UK Challenge (Stormage Cancer) which allowed a consortium of researchers, in particular Ingber and Ferri, to focus on the role of Stroma in the pathology of various diseases, as well as the Montreal Medical Foundation (LF), and an impact subsidy of the Department of Medical Research Programs Defense-Congression (Award # CA200572).
Source:
Journal reference:
PAL, S., and al. (2025). Esophageal adenocarcinoma organic chip derived from the patient: a physiologically relevant platform for functional precision oncology. Journal of Translational Medicine. DOI.org/10.1186/S12967-025-06593-1.