A total of 5,136 people reached the survey. Among these, 4,624 agreed to participate and 4,432 participants completed all the investigation sections and were included in the final analysis. A ventilation of the status of perimenopause and the presence of an absence of 12 months of periods is provided in the table 1. The average age of the participants was 42.6 years (standard deviation (and) = 9.4 years), the majority of respondents declaring being white, European or Caucasians (60.3%).
Analysis 1 – State of the period by the age group
In total, 908 respondents (20.7%) consulted a healthcare professional concerning the perimenopause or menopause. Among the respondents who had seen a health professional, 275 (30.3%) were under the age of 46. The rates of seeing a healthcare professional on menopause or perimenopause were different by the age group (χ2= 803.98, p <0.001), respondents of the age group over 56 with the highest rate of consultations (51.5%) (table 1). Among the respondents who consulted a healthcare professional on menopause, 612 (70.8%) were informed that they were in perimenopause at the time of the consultation. Overall, the status of perimenopause differs by the age group (χ2= 227.79, p<0.001), with the highest rate of confirmed perimenopause received in 51 to 55 year olds (42.6%), Table 1.
Analysis 2 – Symptoms of perimenopause by perimenopause status
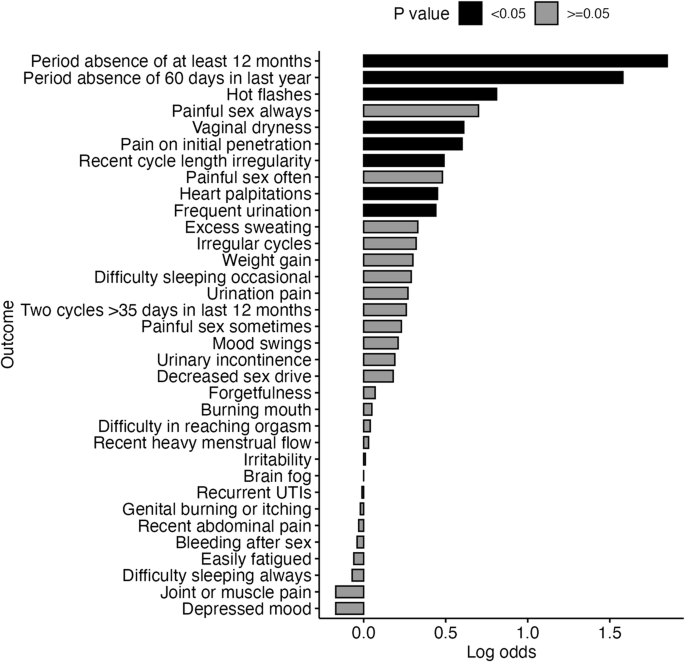
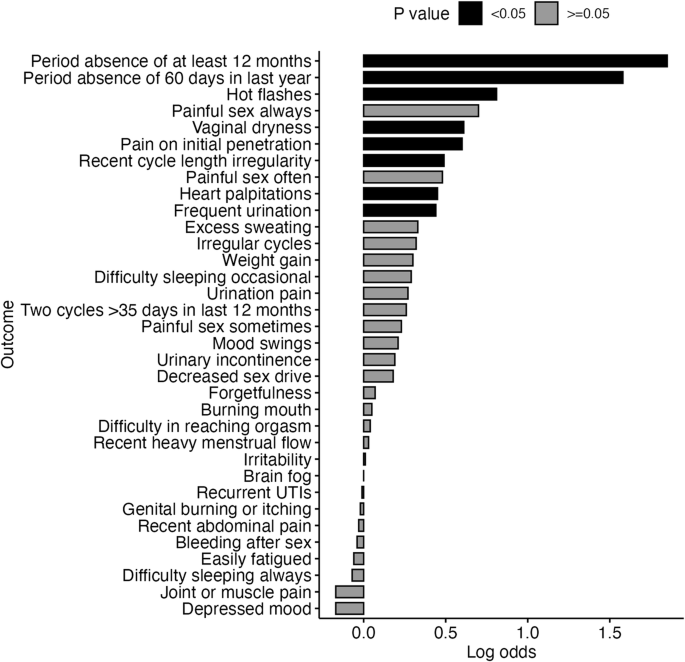
Certain symptoms were more likely to be reported by participants with a confirmed perimenopause as determined by a health professional in relation to those who do not have them. Undefed logarithmic ratings and corresponding confidence intervals (CI) and pThe values of these symptoms were as follows: absence of a period of at least 12 months (logarithmic ratings = 1.85; 95% CI = 1.38–2.38; p<0.001), an absence period of 60 days in the past year (logarithmic ratings = 1.58; 95% CI = 1.19–1.98; p<0.001), heat puffs (logarithmic ratings = 0.81; 95% CI = 0.45–1.17; p<0.001), vaginal dryness (logarithmic ratings = 0.61; 95% CI = 0.25–0.97; p= <0.001), pain on initial penetration during sexual activity (Logarithmic ratings = 0.60; 95% CI = 0.23–0.98; p<0.001), recent irregularity of the cycle cycle (logarithmic ratings = 0.49; 95% CI = 0.11–0.87; p= 0.012), cardiac palpitations (logarithmic ratings = 0.45; 95% CI = 0.06–0.85; p= 0.028) and a frequent urination (logarithmic ratings = 0.44; 95% CI = 0.08–0.82; p= 0.019). Other symptoms did not differ between the two groups, as can be seen in Fig. 1.
Analysis 3 – MR score by age group
We used the MRS to measure symptoms in respondents. The total median score (H= 91.50, p<0.001, η2= 0.02), and the medians of the three domain scores of urogenital symptoms (H= 177.17, p<0.001, η2= 0.04), psychological symptoms (H= 55.70, p<0.001, η2= 0.01) and symptoms of somato-vegetative (H= 209.07, p<0.001, η2= 0.05) differs by the age group. The total MRS score and the Somato-Vegetative domain score were the highest in the age group of 51 to 55, while the score in the psychological domain was the highest in the age group of 41 to 45 years and the score of the urogenital domain was the highest during age groups of 51 to 55 and over 56 years (Table (Table (Table 2).
The MRS score has cuts to indicate the categorical levels of severity of the symptoms linked to menopause. The proportion of respondents falling into the different categories of severity was different according to age, the highest percentage (39.0%) of individuals falling into the severe category being 51 to 55 years. In particular, in this survey, high rates of moderate or serious symptoms are observed even in the youngest age groups, with 55.4% of 30 to 35 years falling into moderate or serious categories (Table 2).
Analysis 4 – MSR and severity scores by perimenopause status
Kruskal Wallis’ tests have indicated that Ms. Total (H= 190.46, p<0.001, η2= 0.04), urogenital (H= 251.82, p<0.001, η2= 0.06), psychological (H= 45.37, p<0.001, η2= 0.01) and Somato-Végetative domain scores (H= 254.98, p<0.001, η2= 0.06) different by the status of perimenopause. The total MRS median score and the psychological domain scores were the highest in the group “premature menopause”. The urogenital median scores were the highest in the groups “I was diagnosed with something else”, “perimenopausic” and “post-menopausic”. The median score in the Somato-Ventative domain was the highest in groups of perimenopausal and premature menopause (table 3).
Dunn post-hoc tests (additional table 2) said the group “did not see a clinician” had a total MRS score lower than that of “non -perimenopausal”, “perimenopause” and “premature menopause groups”.
The “clinician group has not seen” also had a lower urogenital domain score that “non-perimenopausic”, “I was diagnosed with something else”, “perimenopausal groups”, “post-menopause” and “premature menopause”. In addition, the non -perimenopausic group had a lower urogenital domain score that the perimenopausic group.
For the scoring of the psychological field, the group “did not see a clinician” had a score lower than that of “non -perimenopausal” groups, “perimenopausal” and “premature menopause”.
Finally, for the score of the Somato-Ventative domain, the group “did not see a clinician” had a score of symptoms of somato-verteetative lower than all the other groups, and the group “non-perimenopausic” had a score lower than that of the group “perimenopausic”.
When we consider the severity thresholds of categorical symptoms, we have found a global difference in the severity of MRS symptoms in groups of perimenopause status (Table 3). A square chi test between non -perimenopausal and perimenopausal groups did not reveal any difference in the proportion of people in each of the MRS gravity categories between the two groups (χ2= 0.075, p= 0.784). However, there was a higher proportion of individuals in the serious and moderate categories in the perimenopausic group compared to the group “did not see a clinician” (χ2= 149.41, p<0.001).
Analysis 5 – MSR and severity scores by categories of cycle symptoms
The irregularity of the cycle and the amenorrhea are key indicators of the perimenopause. A “persistent” variation of 7 days or more in consecutive cycle length is indicative of early perimenopause, while the amenorrhea of at least 60 days in the past year is indicative of the late perimenopause. The absence of a period for at least 12 months indicates that a person is menopausal. When you use these criteria to classify respondents, we have observed differences in the MRS scores between these groups (table 4). Kruskal Wallace tests have revealed that the total MRS score (H= 118.85, p<0.001, η2= 0.03) and all domain scores (Urogenital: H= 193.65, p<0.001, η2= 0.04; Psychological: H= 45.37, p<0.001, η2= 0.004, Somato-Ventive: H= 183.91, p<0.001, η2= 0.04) Different between individuals with non-cycle symptoms, irregular cycles, an absence of 60 days or an absence of 12 months (table 4).
The total MRS scores were the highest in groups of absence of 12 months, absence of 60 days and irregular cycles with post-hoc tests showing that irregular cycles (Z= 6.35, adj.p<0.001), absence of 60 days (Z= 6.39, adj.p<0.001), or absence of 12 months (Z= 8.69, adj.p<0.001) The group's scores differ from the group of non-cycle symptoms.
The urogenital median scores were the highest in the absence of 60 days and the absence groups of 12 months, the absence group of 12 months different from the absence of 60 days (Z= 6.71, adj.p<0.001), irregular cycles (Z= 4.01, adj.p<0.001) and the group of symptoms without cycle (Z= 13.04, adj.p<0.001), while the absence of 60 days (Z= 6.71, adj.p<0.001) and irregular cycles (Z= 4.81, adj.p<0.001) The groups differ from the group of non-cycle symptoms.
The median psychological score was the highest in irregular cycles and the 60-day absence group, the group of irregular cycles differs from the non-cycle symptoms (Z= 4.15, adj.p<0.001), and the 12 -month absence group (Z= 3.04, adj.p= 0.012).
Finally, the somato-vegetative scores were the highest in irregular cycles, the absence of 60 days and the absence groups of 12 months, the group of non-cycle symptoms with lower somato-vegetative scores than the absence of 12 months (Z = 11.15, adj.p<0.001), absence of 60 days (Z= 8.08, adj.p<0.001), and groups of irregular cycles (Z= 7.17, adj.p<0.001).
The percentages of individuals falling into the categories of severity of the MRS symptoms differ according to the irregularity of the cycle (χ2= 114.91, p<0.001), with more individuals reaching moderate or serious symptom criteria in irregular cycles (76.5%; χ2= 40.23, p<0.001), absence of 60 days (73.7%; χ2= 70.94, p<0.001), or absence of 12 months (χ2= 12.11, p= 0.007) groups that in the group of non-cycle symptoms (60.9%) (table 4).