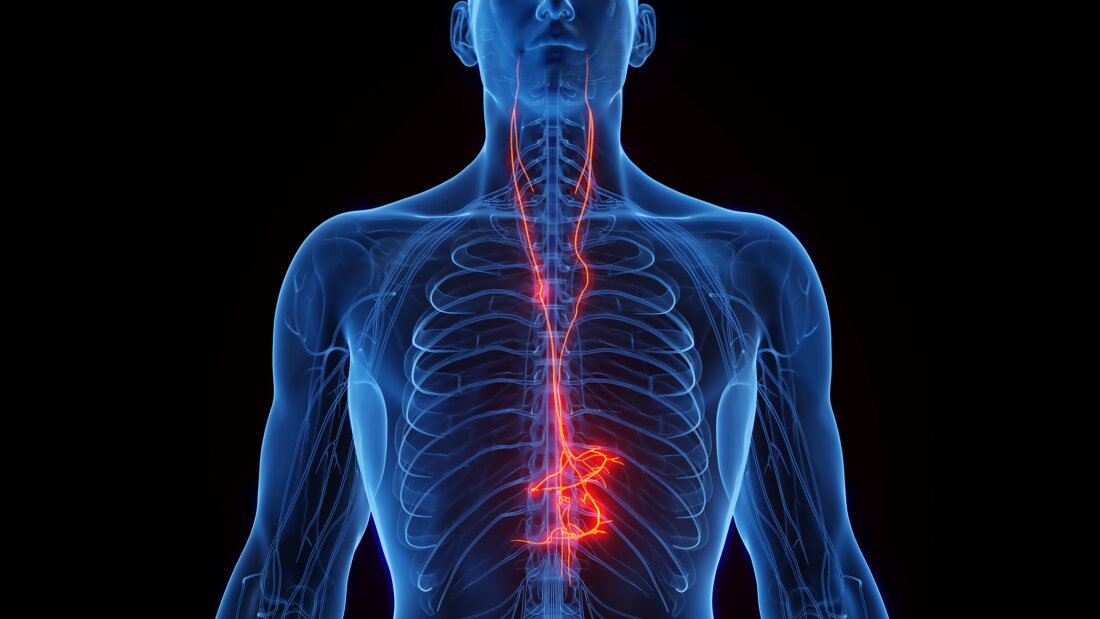
An illustration of the vagus nerve, which is part of the autonomous nervous system.
Sebastian Kaulitzki / Science Photo Library RF / Getty Images
hide
tilting legend
Sebastian Kaulitzki / Science Photo Library RF / Getty Images
Tiny electricity pulses can provide the next major advance in the treatment of diseases such as rheumatoid arthritis.
The impulses would be delivered via established devices that stimulate the vagus nerve, and they are promising in people with arthritis and other autoimmune diseases, including Crohn, and multiple sclerosis.
Currently, autoimmune diseases are generally treated with drugs that remove the immune system. Some of these drugs are given by infusion and can cost tens of thousands of dollars a year. They also increase the risk of a person’s infections.
Stimulation of the vagus nerve could offer a means of increasing or replacing drug treatment, according to doctors.
“Neuronal signals have the capacity to control reflexively the aspects of the immune system that nobody had thought before,” said Dr Kevin TraceyPresident of the Feinstein Institutes for Medical Research of Northwell Health on Long Island.
Tracey co-founded SetPoint Medical, a company that hopes to market a vague nerve stimulation system for autoimmune diseases.
It is still not clear if stimulation of the vagus nerve will be as effective as drug treatment, says Dr Andrew KoA neurosurgeon from the University of Washington in Seattle which has implanted set point stimulators in patients with rheumatoid arthritis as part of a study.
“The drugs work, but they sometimes don’t do it, and you can have side effects,” said Ko. “In these cases, there are advantages to examining the devices.”
Ko notes that the stimulators of the valued nerve implanted are already approved for certain patients with epilepsy and depression. The devices that stimulate the brain of people with Parkinson’s disease have proved to be “better than drugs” to reduce symptoms, he said.
Rheumatoid arthritis, which affects approximately 1.5 million people in the United States, is about to become the first autoimmune disease treated with electrical pulses sent by the vagus nerve.
A device Made by SetPoint Medical is being examined by the US Food and Drug Administration, which is likely to make a decision by the end of 2025.
The agency’s examination will include a 2024 study of 242 patients. He find These 12 weeks of stimulation with the device have considerably reduced both the symptoms and the progression of the disease. In addition, damage to their joints occurred more slowly and the levels of inflammatory protein have dropped dramatically.
An wandering nerve that connects the brain and the body
The bond of the vagus nerve with the immune system was discovered by accident over 20 years ago.
Kevin Tracey of Northwell and a team of researchers gave rats an experimental medication intended to prevent inflammation in the brain. To their surprise, it also eliminated inflammation in the body.
The reason has proven to be a signal sent from the brain to the body’s immune system.
“We realized that the signal moved into the vagus nerve and that the vagus nerve was like the brake pipes in your car,” explains Tracey. “It was the brakes on inflammation.”
Tracey says that the realization has led to a question: “Can we make devices that turn on the brakes, then treat patients with excessive inflammation?”
It would take decades of research to get there.
The vagus nerve is actually a pair of nerves, right and left, which connect the brain to internal organs, including the heart, lungs, liver, intestine and spleen.
“It is the only nerve of your body if you cut it on both sides, you will die,” says Tracey.
A large part of contemporary research on the vagus nerve was carried out at the FEINSTEIN Institute of Bioelectronics Medicine, one of the Tracey Institutes supervised. Dr Stavros Zanos is in charge of a team that has mapped the human vagus nerve, which is often compared to a signal transport superhigle throughout the torso.
During a visit to his laboratory, Zanos holds a transparent tube containing a foot or two of fabrics in the shape of a white cord slightly finer than a pencil.
“It is most of the vagus nerve from the brain to the neck half the distance through the chest,” he said.
Then he shows me what a transverse cut under a microscope looks like.
“It’s like a slice of a cucumber,” he said. “You see all these tiny green spots, thousands and thousands of them? These are individual fibers.”
The bundles of the right and left vagus nerve each have more than 100,000 of these strands.
“Many fibers inform the brain of the inflammatory state of the whole body,” said Zanos.
Feinstein researchers have listened to these fibers in animals and have even developed a system that transforms traffic along the audio wave in real time.
This allows them to hear how inflammation of the body changes the signals to go to the brain.
Sangeeta Chavan plays a recording of an experience. At the beginning, there is a constant thrum after the rhythm of heart rate and breathing, but when the researchers inject a substance which causes inflammation, the sound becomes like popcorn fallen into hot oil.
“When inflammation occurs, molecules activate signals that go up the vagus nerve,” explains Tracey.
And it’s only half of the story.
Electric impulses activate a reflex that makes the brain produce another set of signals that returns in the vagus nerve.
These are the brake signals, the Tracey team discovered decades earlier. They stamp the immune system so that inflammation does not become uncontrollable.
The signals do so by telling certain immune cells to stop producing inflammatory proteins called cytokines.
“What we have discovered is that the signals of the vagus nerve deactivate the production of cytokines in the spleen”, an organ that plays a major role in the immune response.
Then, Tracey’s team learned to stimulate the vagus nerve in a way that activates the anti-inflammation reflex.
This allowed SetPoint Medical to develop an implantable stimulation device.
“This is the size of a large pill, a very large multivitamin,” said Ko, adding that it is similar to the vague nerve stimulators approved by the FDA that it implants in patients with epilepsy.
The point of view already looks beyond patients with rheumatoid arthritis. The company has launched trials on its stimulation device in patients with multiple sclerosis and Crohn’s disease.


