The study of the CB1 receptor has implications for the treatment of chronic pain.
A research team financed by the National Institutes of Health (NIH) has developed a drug that is promising in the treatment of acute and chronic pain. The drug, known as VIP36, targets the cannabinoid receptor of type 1 body (CB1). It turned out to be effective in three different animal models of pain and does not seem to cause the harmful side effects that have frustrated other efforts to target CB1. These results strengthen understanding of the design of safer and more effective drugs targeting cannabinoid receivers and constitute an important step towards the development of new non -addictive treatment for pain.
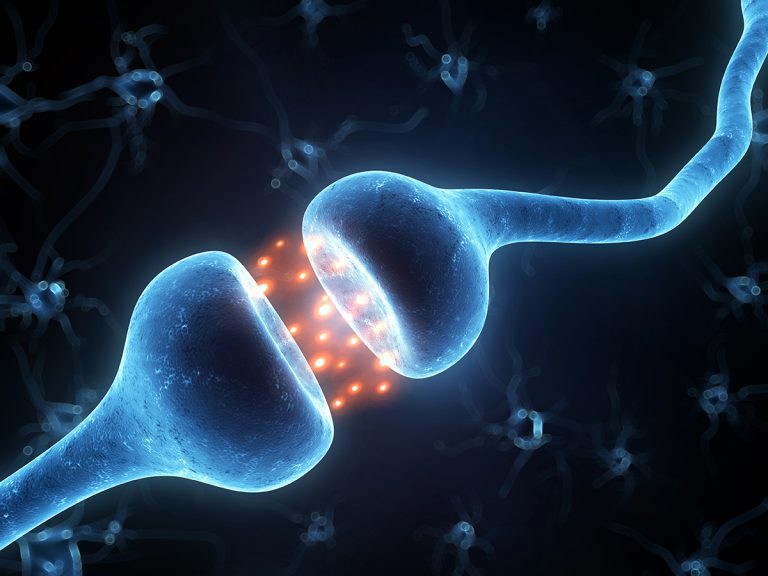
CB1 receptors can be found throughout the body and are particularly dense in brain pain circuits. They have long been considered a potential target for the treatment of non -opioid pain; However, previous attempts to target this path were noted with two challenges. First, repeated exposure to a drug leads to tolerance that limits its effectiveness. Second, the dose necessary to reduce pain in the periphery tends to be high enough for the medication to enter the central nervous system. In humans, this can cause undesirable changes in mood, cognition or emotional state.
To overcome these problems, the researchers have exploited the computer modeling of the CB1 receptor with design molecules which interact better with CB1, a bit like a key adjustment in a lock. The newly designed drug, VIP36, is more “peripheral” limited “compared to previous drugs, which means that much less flees in the central nervous system where it can cause undesirable side effects. VIP36 also interacts with CB1 differently from the treatments tested previously and in a way that reduces tolerance.
CB1 is part of a large class of receptors known as receptors coupled with G proteins, which are involved in countless functions throughout the body, in particular the smell, vision, mood regulation, immune system responses, responses from the autonomic nervous system such as blood pressure and heart rate, and growth and metastases of certain tumors. In addition to their implications in pain care, the results of this study could also help stimulate the design of other drugs that target similar receptors involved in other conditions.
This research was funded by NIH Help end the long -term dependence initiativeOr NIH Heal Initiative®, an effort on the level of the NIH which seeks to accelerate scientific solutions to the epidemic of overdose, including the disorders of the use of opioids and stimulants, and the crisis of chronic pain.
WHO
Julia Bachman, Ph.D., Heal Program Manager, NIH
Article
Rangari Va et al. “A cryptic pocket in CB1 leads to peripheral and functional selectivity” Nature. March 5, 2025. Doi: 10.1038 / S41586-025-08618-7
About the National Institute of Neurological Disorders and Cerebral Vascular Accidents (Ninds): Zero is the country’s main donor on the brain and the nervous system. Ninds’ mission is to seek fundamental knowledge about the brain and the nervous system and use this knowledge to reduce the burden of neurological diseases.
On the National Institutes of Health (NIH):The NIH, the country’s medical research agency, includes 27 institutes and centers and is a component of the American department of health and social services. NIH is the main federal agency that leads and supports basic, clinical and translational medical research, and studies the causes, treatments and remedies for common and rare diseases. For more information on NIH and its programs, visit www.nih.gov.