The American Ministry of Labor has noted a generalized non-compliance and violations of the federal law in the way in which health regimes and insurers cover mental health care, conclusions that reflect A recent propublica survey.
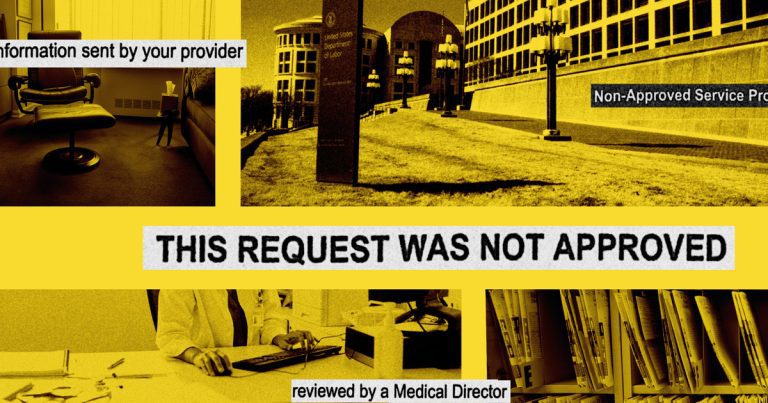
The health regimes and the companies that administer them excluded key behavioral treatments, such as therapies against drug addiction and autism, and have proposed inadequate networks of mental health providers, according to a 142 -page document. report Posted on January 17 in collaboration with the Treasury and Health and Social Services departments.
The report, which agencies are required to regularly submit to Congress, also details the results of secret surveys with more than 4,300 mental health care providers listed in insurance directories and reveals that “alarming proportion” was “insensitive or inaccessible”. Such truffled errors plans, commonly known as ghost networks, make patients more difficult for patients to obtain the treatment they need, said Propublica. previously found.
Since 2021, the Ministry of Labor has looked into the violations of health plans which serve more than 7 million people, according to the report. The agency has endeavored to remedy the problems by seeking to modify the provisions, policies and procedures of the regime, as well as ensuring that the requests wrongly refused to be paid.
But the report recognizes that even if the regimes and the insurers have made certain progress, they continue to be lagging behind. For example, federal officials have written that insurers worked faster to solve the problems of their regimes once they had been identified, but that those responsible had not noted sufficient improvement overall.
The report examines the application and implementation of the federal law on mental health parity and equity in drug addiction, which requires that health insurance plans provide the same access to mental health care than medical care. Last week, the same day of publication of the report, the staff of the department told Propublica that the agency was investigating problems related to our reports.
Good journalism makes the difference:
Our independent and non -profit editorial staff has only one mission: to ask the powerful accounts. Here’s how our surveys take place Stimulate a change in the real world:
We try something new. Was it useful?
Propublica spent last year investigate how insurers intervene with mental health treatment, including using aggressive tactics that push therapists out of the network; deploy a algorithmic system to limit the coverage; create ghost networks; cut access to Treatment for autistic children; rely on doctors whose judgments have been criticized by justice; and using patients progress to justify refusals.
The Ministry of Labor regulates insurance plans of approximately 136 million Americans benefiting from health coverage through their employer and is responsible for enforcing federal protections concerning their mental health complaints. Federal regulators have struggled to keep the insurance companies responsible for their unjustified refusal of mental health coverage, partly due to staff and budgetary constraints.
The agency has repeatedly asked the congress of additional funding and, in its most recent report to the congress, wrote that it found itself with an investigator for 13,900 regimes which it regulates, which represents a higher workload that in previous years. Certain temporary funding is exhausted in September, and their “complete exhaustion will probably have catastrophic effects” on its implementation capacities, according to the report.
Timothy Hauser, deputy deputy assistant secretary, said in an interview on the day of publication of the report that the agency was investigating the surveillance and management of doctors hired by insurance companies that repeatedly refuse health coverage mental to patients – and could open additional surveys. .
Hauser, who has been working at the agency for more than three decades and remains in the new administration, said that the agency is studying how insurers use and supervise the doctors on which they rely to carry out cover exams and if These doctors examine cases in a fair and impartial way “. Propublica reports have raised serious concerns about these questions.
Last month, Propublica examined how insurance companiesincluding Unitedhealth Group, Cigna and Blue cross and blue shieldcount on doctors to make crucial decisions regarding the approval or not of mental health coverage, even after the courts criticized their judgment. The judges judged that by refusing such a coverage, the insurers had violated the federal law and acted in a way which was “confusing“”deceitful“And even”dishonest. “
Some insurers and doctors, according to the judicial archives, have engaged in “Selective readings“Medical proof,”look down»To medical opinions which opposed their conclusions, and made Critical errors In their criticisms sometimes contradicted by the medical records they had said to have read.
Hauser said he could not comment on specific investigations, but said that agency officials had discussed the history of Propublica, who, according to him, “will have an impact on the questions we ask” and The “approaches we adopt”.
At least one investigation in the past has resulted in the dismissal of a doctor and the external examination organization for which he worked, said a spokesman for the Ministry of Labor.
The whole country’s insurance companies rely on doctors working on their behalf to determine if the treatment sought by patient doctors is medically necessary. If they determine that this is not the case, they recommend refusing coverage, which can leave patients in crisis and without the treatment they need. In some cases, these decisions have had fatal consequences.
“This is supposed to be done with impartiality and without having been structured so as to encourage doctors to favor the refusal of complaints rather than acceptance of complaints,” said Hauser. “Likewise, doctors and service providers should not be selected because of their propensity to refuse complaints. »»
United, Cigna, Blue Cross and Blue Shield immediately responded to requests for comments, but said in the past that they employ approved doctors to carry out exams and ensure that doctors make appropriate coverage decisions . Companies said they made regular audits of doctors’ decisions, that they offered mentoring and coaching opportunities and that they undertook to provide patients with access to safe, effective and quality care.
Hauser said he was struck by The story of Emily Dwyerwhich was presented in an article by Propublica examining the role of corporate psychiatrists. She was 15 years old and suffered from severe anorexia – she arrived in a residential treatment center bearing the jeans of her 8 -year -old sister – when United Healthcare refused her coverage.
United arises that three separate doctors had examined his case. The Dwyers brought a legal action and lost, but appealed to the 5th Court of Appeal of the United States, which canceled this decision and pronounced unanimously in favor of the family. In a very critical opinion, the judges wrote that the letters of refusal issued by the three doctors were “not supported by the underlying medical evidence”. In fact, the court concluded, this information was “contradicted by the file”.
Dwyer, who was delighted to learn the investigation carried out by the agency, said that she hopes that she will lead to a “substantial action”.
“I would never have thought that our story would be part of it,” she said. “I find it incredible that the Ministry of Labor is interested in this issue and investigates insurance doctors. But I also hope that they will look beyond the actions of individual doctors and will be interested in deeper problems linked to the more systematic functioning of insurance companies. ”