Design, sampling and parameterization of methods
A convergent parallel mixed methods design was used to evaluate the University of Greenville Medicine (USCSOMG) HL curriculum, including their Family Medicine Graduate Medical Education (GME) program through the Greenville Family Medicine Residency (FMRGVL). Survey participants were USCSOMG students and FMRGVL residents. The sampling frame included a total of 432 individuals, 113 first-year medical students (M1), 110 second-year medical students (M2), 98 third-year medical students (M3), 93 fourth-year medical students (M4), and 18 residents in family medicine. Learners were recruited to participate via classroom presentations, emails/listservs, short text messages, and GroupMe messaging. To be included in the study, individuals had to be current learners in either program. Five current faculty members from the programs conducted interviews. Faculty members were identified using a purposive sampling method and chosen due to the presence of some form of HL or HL-related concepts in their program, as identified by another USCSOMG faculty member. Both USCSOMG and FMRGVL utilize interprofessional education with faculty members from a variety of disciplines beyond clinical medicine and provide training in HL and patient communication.
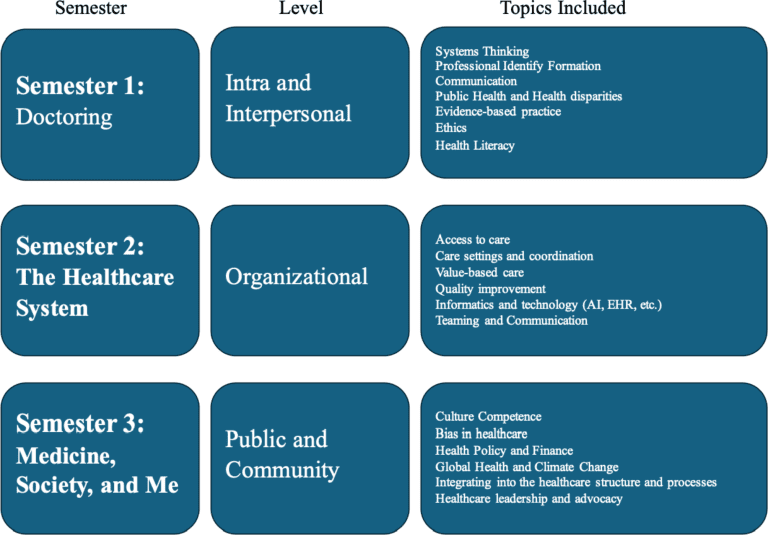
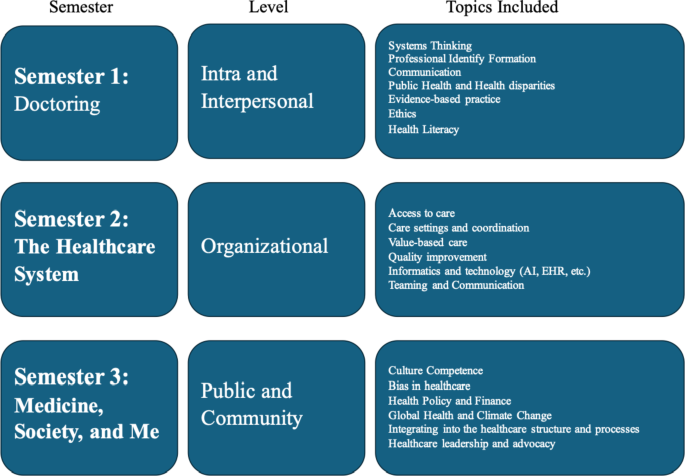
USCSOMG includes HL training in its first-year Integrated Practice of Medicine (IPM) program. IPM courses are taught throughout all four years of medical school and in small groups, with year-long courses during the first two years and one- to four-week sessions in the third and fourth years (17). USCSOMG is updating its curriculum to improve patient-centered care, adding semesters on medicine, the health system, and societal aspects of medicine (Fig. 1). First-year students take a course on HL and are tasked with creating brochures about HL using simple language. Brochures should include the definition of HLH, the impacts of HL on health outcomes, how to assess HL, how to help patients with HLH, information on the retraining method, statistics on HL and strategies that health systems can put in place to address this. help patients with HLH. IPM and clinical faculty also strive to integrate training on motivational interviewing, patient feedback, medication reconciliation, and other HL interventions throughout their courses under the form of role-playing, simulated patient interactions and discussions. First-year students also benefit from EMT internships, allowing them to have hands-on experience with patients of varying levels of HL before entering the clinical environment.
In the FMRGVL, videos of residents’ interactions with patients are reviewed using the University of Washington Patient-Centered Observation Form (18). This form allows the instructor to assess how well the resident addresses the biopsychosocial aspects of patient care and uses good communication techniques, including patient learning. The program also hosts Equity M&Ms, which aim to educate residents on concepts related to health equity and encourage discussion about HL, learnings from patients and other contributors to health care affected by the determinants social health (19).
Measures
The survey (Appendix 1) assessed medical learners’ previous and current HL training, their comfort and knowledge of HL concepts, and their opinions about HL education in medical schools. The survey was adapted from a measure developed by Mackert and colleagues (16) used to evaluate the long-term effects of HL training for medical students (15) and components of the AHRQ Health Literacy Universal Precautions Toolkit (9). General demographic data was not included to preserve the anonymity of survey respondents. Question types included multiple choice, ranking, and open-ended responses.
The faculty interview guide (Appendix 1) contained open-ended questions aimed at gathering information about the faculty member’s role at USCSOMG, as well as information and opinions about their explicit and latent HL program.
Statistical procedures and analyzes
Anonymous online surveys created in Qualtrics were sent using the same recruitment methods. Survey collection took place from January 17, 2024 to March 1, 2024, and several text and email reminders were sent to students to encourage participation during the collection period. A $5 Starbucks gift card was offered for participation. A snowball sampling method was used to reach eligible participants. The survey QR code was shared with learners by some USCSOMG faculty members during classes and via email. For a survey to be considered “complete,” participants had to answer all of the initial categorical questions and at least one of the Likert scale questions. 84 people responded to the survey and 71 people completed the survey.
Five interviews were conducted with faculty members who include HL in their curriculum to assess their curriculum and their opinions on barriers to addressing HL. Interviews were conducted on Microsoft Teams and lasted 20 to 45 minutes, with an average length of 31 minutes and a standard deviation of 8.7 minutes. Interviews were recorded and transcribed, and oral consent was obtained before each interview. Interview data were digitally labeled and deleted at the end of the study.
Thematic analysis was the primary qualitative method for analyzing the USCSOMG faculty interviews and open-ended survey responses from medical learners. Interview transcripts and open-ended responses were imported into Microsoft Word, and codes were generated using various formatting styles (e.g., bold, underline, italic) to highlight relevant data segments for the evaluation of the HL program. The codes were then grouped into themes and relevant quotes within each theme were extracted.
RStudio, version 4.3.2, with alpha set at 0.05, was used to analyze the results of the quantitative survey. Survey respondents were grouped into preclinical (M1-M2 students), clinical (M3-M4 students), and residents. The Likert scale questions were grouped into Strongly Agree/Agree, Neutral, and Disagree/Strongly Disagree. Some categorical questions were also grouped together, for example, 0-3 hours, 4-10 hours, and 11-15+ hours spent on social health education and none/little or none, sometimes a decent amount/almost always use social health interventions in real-world situations. global patient interactions. Ranking questions were dichotomized, for example ranking 1/2 or any other ranking. All percentages were calculated using the number of responses to each specific question in the denominator to fill in missing responses.
Descriptive statistics were performed for categorical and continuous variables. Kruskal-Wallis tests were performed to determine differences in response to the Likert scale and ranking questions between the preclinical, clinical, and residency groups, and Shapiro-Wilk tests were used to test normality. The data violated the assumptions necessary for parametric tests; therefore, nonparametric tests were used.
The University of South Carolina Institutional Review Board has determined that this project is exempt from review (#Pro00132250).