Humans today are living longer than everbut how many of those extra years were spent in good health?
An in-depth investigation of data covering 183 member countries of the World Health Organization has now confirmed what some scientists fears: While years are added to most people’s lives, a healthy life is not added to most people’s lives.
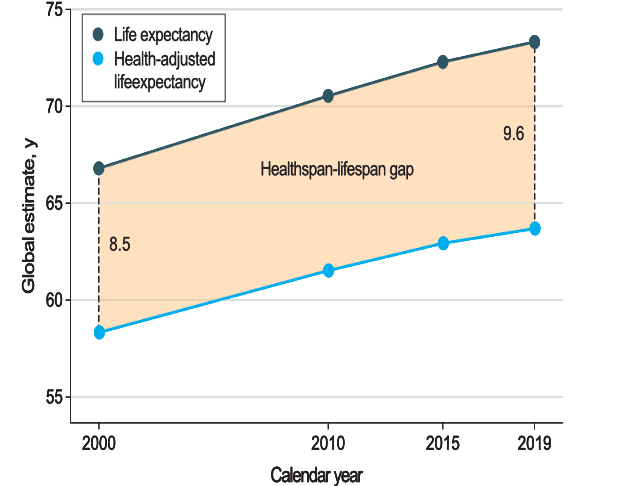
Mayo Clinic researchers found that in 2019, people worldwide lived 9.6 years of life with a disability or illness, a 13% increase from 2000.
During the same period, global life expectancy increased by 6.5 years, while health-adjusted life expectancy increased by only 5.4 years.
In the United States, the gap between lifespan and “lifespan” is particularly widening.
Between 2000 and 2019, life expectancy in the United States increased from 79.2 to 80.7 years for women and from 74.1 to 76.3 years for men.
However, after adjusting for additional years of healthy life, lifespan increased by only 0.6 years among men. And for women, even if health-adjusted life expectancy fluctuates slightly over time, in 2019 it corresponds to the figure observed in 2000.
This growing gap means that if an American woman lived to the expected age of 80.7, the last 12.4 years of her life would, on average, be affected by illness or disability.
According to public health researchers Armin Garmany and Andre Terzic, the gap between lifespan and health in the United States is 29% higher than the global average.
“Data shows that gains in longevity do not correspond to equivalent gains in healthy longevity. Getting older often means more disease-laden years of life,” said Terzic, a cardiovascular health researcher at the Mayo Clinic.
“This research has important practical and policy implications by calling attention to a growing threat to the quality of longevity and the need to close the gap between health and lifespan.”
The findings are consistent with previous studies from around the world, which generally consider one nation at a time and suggest that even if women tend to live longer that men, too accumulate more years of life in poor healthmainly due to chronic health problems.
In light of these trends, WHO recently introduced a new measure known as healthy life expectancy (HALE) to attempt to measure the burden of disease and disability among older people, particularly after age 60.
In 2020, the WHO and the United Nations declared a 10-year global action plan. In 2022, those responsible wrote that to “ensure older people are not left behind, there is an urgent need to strengthen measures and close data gaps”.
Mayo Clinic researchers have now answered that call.
In a review of the last two decades, Garmany and Terzic have highlighted “a chasm between progress in longevity, a traditional measure of life expectancy, and healthy longevity, a contemporary indicator of the quantity and quality of life.”
The growing gap between these two measures is now confirmed as a global trend and, although it is a universal problem, it will need to be addressed in a multifaceted way, from country to country and between different groups of people.
For example, the gap between life expectancy and healthy span is particularly pronounced among women, who tend to bear a greater burden of noncommunicable diseases, such as musculoskeletal, genitourinary, and neurological diseases. , later in life.
The largest health and lifespan gaps were observed in the United States (12.4 years), Australia (12.1 years), New Zealand (11.8 years), United Kingdom (11.3 years) and Norway (11.2 years).
Meanwhile, the lowest gaps were observed in Lesotho (6.5 years), Central African Republic (6.7 years), Somalia (6.8 years), Kiribati (6.8 years) and Micronesia ( 7.0 years).

Since poor health was analyzed using an overall measure of illness and disability, the researchers say the next step is to dig deeper, determining which groups of people suffer most over the course of their final years and how we can best help them age with dignity. .
“The growing gap between lifespan and lifespan is a global trend, as documented here, and highlights the need for an accelerated pivot toward proactive care systems focused on well-being,” the two authors conclude.
The study was published in Open JAMA Network.


