Béenzeisler et al.1 Show how federated access to 7.9 million data sets representing 2 million patients allows the secondary national use of emergency medicine files while joining national and European law. This is an exemplary use case and an early overview of the place where Germany and Europe are heading to strengthen research capacity on health and confidence of citizens.
Emergency service national register
The national register of emergency service data is a federated research infrastructure. It is a pillar and operated on in the German network of university medicine (see below) and provides federated access to standardized and structured electronic health files of emergency rooms1,,2,,3. Individual informed consent can be given back because the files remain stored locally, thus adhering to general medical confidentiality and data confidentiality legislation. Researchers can file requests with a committee for using and accessing data for examination and approval to enforce ethical and scientific standards. After the authorization, the data is collected and analyzed in a trusted research environment. Béenzeisler et al.1 Must be congratulated not only for the high level of structured data collection coordinated in their system, but perhaps even more for having succeeded in taking up the challenge of governance of decentralized data, where each of the 16 German federal states has its own medical regulations and general processing of data combined with the European provisions of general data protection regulations (GDPR). The alternatives to this complexity would be the Canadian province of Alberta, where the health files of the entire population are stored in a provincial electronic health file in a structured and coordinated manner, allowing easy implementation of specific care pathways and decision -making tools at the provincial level4,,5,,6 or the Emergency Care Data of the Kingdoms in the United Kingdom (ECD)7.
Rapid digital transformation of the German health system
Germany provides health care to its eighty-three million citizens thanks to the first global social insurance system introduced in 1883 by the German Chancellor Otto Von Bismarck, who laid the foundations for the current statutory health insurance system covering most Germans and inspired by other health systems since. Its origins date back to the Middle Ages when guilds and selected companies have assumed responsibility to finance medical and nursing care for their members and employees8.
Today, some 1900 hospitals and 430,000 doctors take care of the population of the country, which costs more than a billion billion dollars a day, that is to say more than 10% of the gross domestic product in Germany. Like all the countries of the seven of the seven (G7) and the countries of the Organization for Economic Cooperation and Development (OECD), Germany is struggling to increase health spending. Germany has lagged behind when the United States, Canada and the European Nordic countries have decided to deploy digital technologies to meet the challenge in the late 90s and at the start of this century. The recent pandemic was an awakening exposing the weakness of Germany when crisis management has been hampered due to the lack of centralized health data systems to coordinate resources nationally requiring a manual transcription of fax messages. On the other hand, other jurisdictions such as the Canadian province of Alberta, with a provincial electronic health file system, exploit an entirely digital emergency control center9.
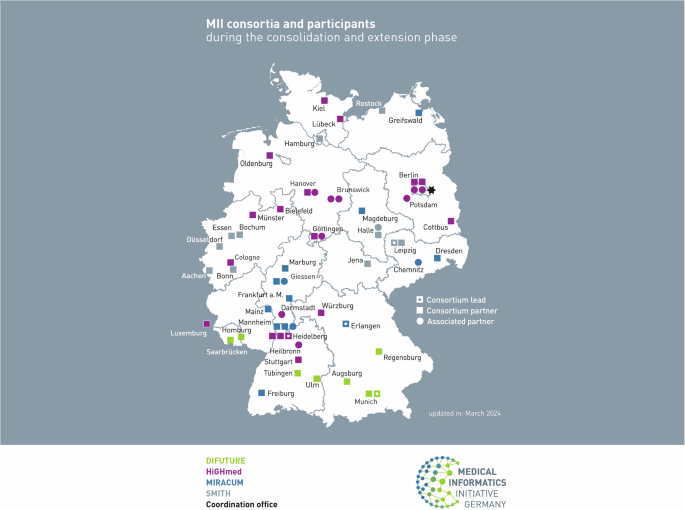
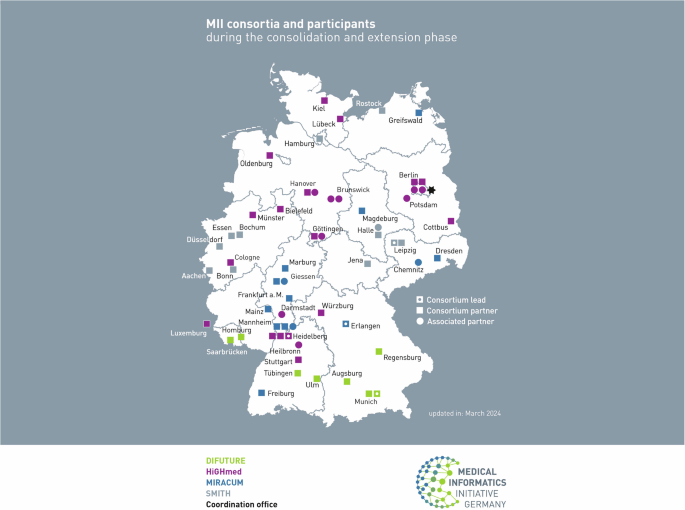
The first initiative aimed at overcoming this problem was launched in 2020 as a network of university medicine, a national network of university medical centers for crisis management and coordinated COVVI-1910 research. Its mission has evolved to promote clinical research and knowledge transfer of knowledge comparable to research strategy of research on research on health research in Canada for patient research11. Above the same time, Germany launched its 500 million medical computer computer science financing system to make the data in secondary life sciences more accessible to strengthen biomedical research and improve patient care. The medical initiative of IT unites stakeholders in university medicine and all research institutions, companies, payers and patient defense groups12 (Fig. 1).
The biggest boost, however, comes from the launch of this year of the National Health Data Lab13. It manufactures pseudonymized health data of all people (around 75 million or approximately 90% of the German population) provided in the German statutory health system available for research purposes. The strategic objective is to provide effective and effective medical care thanks to the full digitization of the entire health system. Additional support initiatives are the strategy of artificial intelligence of Germany (AI)14including both an online platform for learning systems15where experts in the academic world, industry, policy and civic organizations discuss development and responsible use, as well as a national artificial intelligence observatory16 Monitoring the impact of AI in the workplace and on the company.
An important step for the European Health Data Espace (DSE)
Recent substantial investments in Germany in the digital transformation of its national health system mark an essential step for the European Health Data Espace (EHDS) launched this month. The European Union (EU) appreciates the importance of significant use of transnational data. The DUHD aims to improve access and control of individuals on their personal electronic health data while allowing the use of secondary data for public interest, political support and scientific research. It includes the establishment of a harmonized legal and technical frameworks for electronic health file systems17.
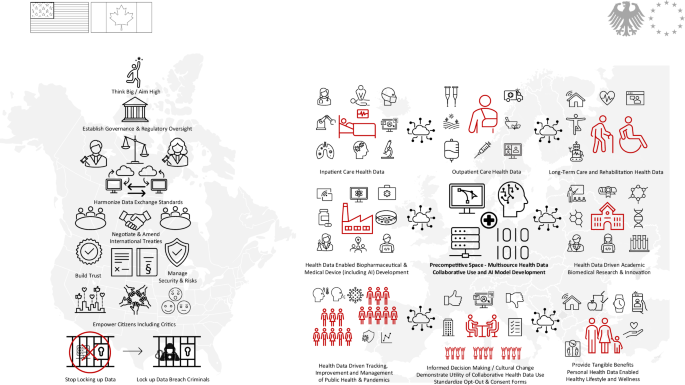
Impact on North America and prospects for the world
The United States has created and shelters some of the most emblematic resources for research in life sciences, such as the entirely digitized medical library or the International Health Organization (HL7) standardizing interoperability3 And also most of the largest digital technology companies in the world, including those focused on artificial intelligence. Canada has been an early adopter of digital health, including telemedicine, to offer health care through its vast geography. It was the first country to have a national AI strategy18 and deeply advanced depth learning and learning strengthening.
The digital breed of health and life sciences will ultimately be determined by access to health data representative of the population to train reliable models. This is where countries like Germany and the EU open the way now. All countries are invited to follow their initiative and are invited to join. European Countries not of the EU, such as the United Kingdom (United Kingdom), have developed national strategies for the sharing of federated health data such as their health data research gateway (HDR UK), the Federated Data Platform for National Health Data (NHS FDP), the NHS Artificial Intelligence Laboratory and the Associated UK BIOBANK. The United States and the EU have introduced the data confidentiality framework with cross-border data transfer agreements19. Canada has recently joined Horizon Europe, with its strong orientation in life sciences and technology, and has also taken measures to sharing transnational data20. However, despite efforts such as the Data for Health multinational initiative, their objective was mainly on privacy21 (Fig. 2).
Health data (relevant) and life sciences (linked) do not only come from primary health care or research environments. Instead, stakeholders in health care, academic world, industry, society and government all contribute to it. The collaborative use of data on health and multisource life sciences to allow digital innovation requires cultural change, the establishment of confidence between all stakeholders, the harmonization of technical and legal standards, aligned regulatory processes and a rationalized exchange platform for citizens, researchers, developers and innovators. Reproduced with permission.
Béenzeisler et al.1 The work impressively demonstrates the potential for sharing collaborative health data and how to master complex legal constraints. Global health, life science research and biomedical industry would benefit most of them if more nations and continents followed the national and continental health data spaces in Germany and Europe for the greatest good of humanity.