The quality of housing is a fundamental determinant of health, but efforts to quantify the conditions of mediocre housing at the national level have been limited. A new study Combines this gap by introducing the metric of housing quality (HQM). Developed by researchers from the Johns Hopkins Bloomberg School of Public Health, including Craig Pollack.
The HQM was developed using MicroData from the American Housing Survey 2021 as well as the 2018-2022 American community survey. The metric assesses the quality of the accommodation at the census sectors in three key areas:
- Physical insufficiency – Structural deficiencies, including plumbing problems, exposure to mold and poor insulation.
- Housing costs load – The proportion of household income spent on housing, which can limit financial flexibility for essential needs such as health care and nutrition.
- Perception of the poor district – indicators such as abandoned buildings, high vacuum rates and crime reports that influence residents’ well-being.
To assess the validity of the HQM, the researchers examined its association with health measures at the level of the derived area of the set of places, which provides small area estimates of auto -declared health results. The study focused on three key indicators: fair or mediocre general health, poor mental health and poor physical health. Regression models have been used to assess the relationship between HQM scores of census leaflets and these health measures in non -adjusted analyzes and models controlling potential confusion factors.
The study revealed that higher HQM scores – indicating poorer housing conditions – were significantly associated with negative self -declared health results. More specifically, the census sectors with higher HQM scores had higher proportions of adults signaling fair or mediocre general health. In addition, poor mental health results were more widespread in census sectors with worst housing conditions, and poor physical health was significantly associated with higher HQM scores. These associations have remained significant even after adjustment for other factors, highlighting the independent impact of the quality of housing on the health of the population.
These results support the pressing link between health and housing. Poor housing conditions can expose residents to environmental risks, including mold, vermin and inadequate heating, which are all precursors for long -term conditions such as asthma, cardiovascular disease and respiratory diseases. Financial charges due to high housing costs can also trigger pressure, food insecurity and delays in the search for medical care. The perceptions of the neighborhood also play a role in health results. The presence of abandoned buildings and signs of negligence can contribute to anxiety, depression and an overall drop in mental well-being.
According to Pollack, “the accommodation is more than a simple place to live – it shapes people’s health in a way that goes beyond the walls of their house. The HQM allows us to enter the broader impact of the quality of the accommodation and its role in the training of health disparities. »»
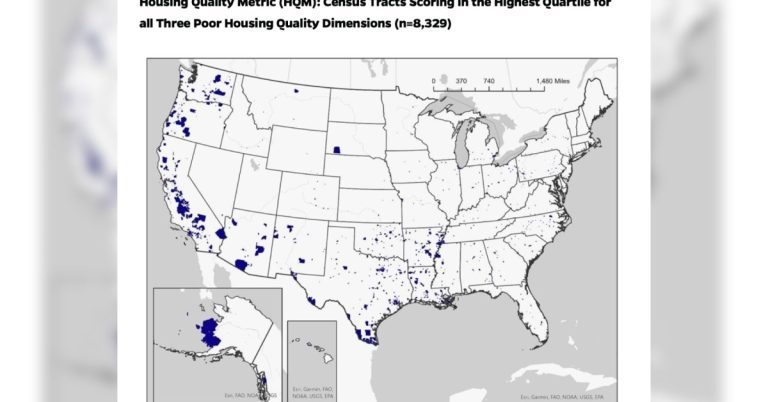
The introduction of HQM has important implications for efforts of public health, research and intervention policy. Political decision -makers and health officials can use this metric to identify high -risk communities where poor housing conditions can stimulate health disparities, strategically allocate resources to improve housing conditions and reduce health risks and monitor changes over time to assess the impact of housing policies and interventions.
Unlike previous measures focusing solely on the affordability of housing or structural insufficiency, the HQM captures a more complete image of the quality of the accommodation, incorporating physical, financial and neighborhood factors.
The HQM is available to download and use here.