Digital health technology is progressing at lightning speed, but innovation requires a human touch to ensure that everyone benefits from advances, according to speakers at the first ASU digital health summit on Friday.
Digital health refers to technology such as portable devices, remote charts, artificial intelligence and the management of all personal data produced.
“If we are only counting on technology, we are not going anywhere,” said Michael Yudell, temporary dean and professor at the College of Health Solutions at Arizona State University.
“We need social-behavioral scientists to understand the impact of these technologies, how they meet with different types of communities and how they will help or perhaps harm the most vulnerable of us.”
The one-day event, which was held on the Campus in downtown Phoenix, covered a range of subjects, including examples of how digital health innovations help people with dementia , why the creation of a “digital twin” can improve health care and how to make these technologies everyone benefits. The summit was sponsored by the College of Health Solutions, the new asu Roybal Center for the elderly living alone with a cognitive decline and the Google government.
Here are some protruding facts:
The elderly want a technology
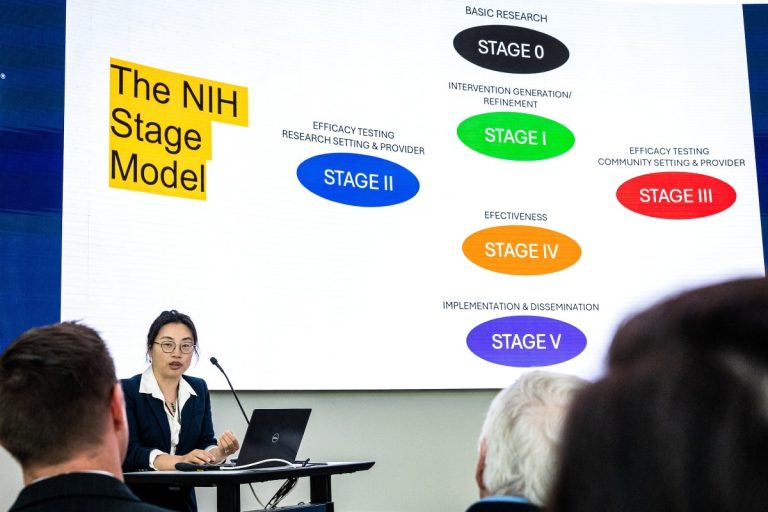
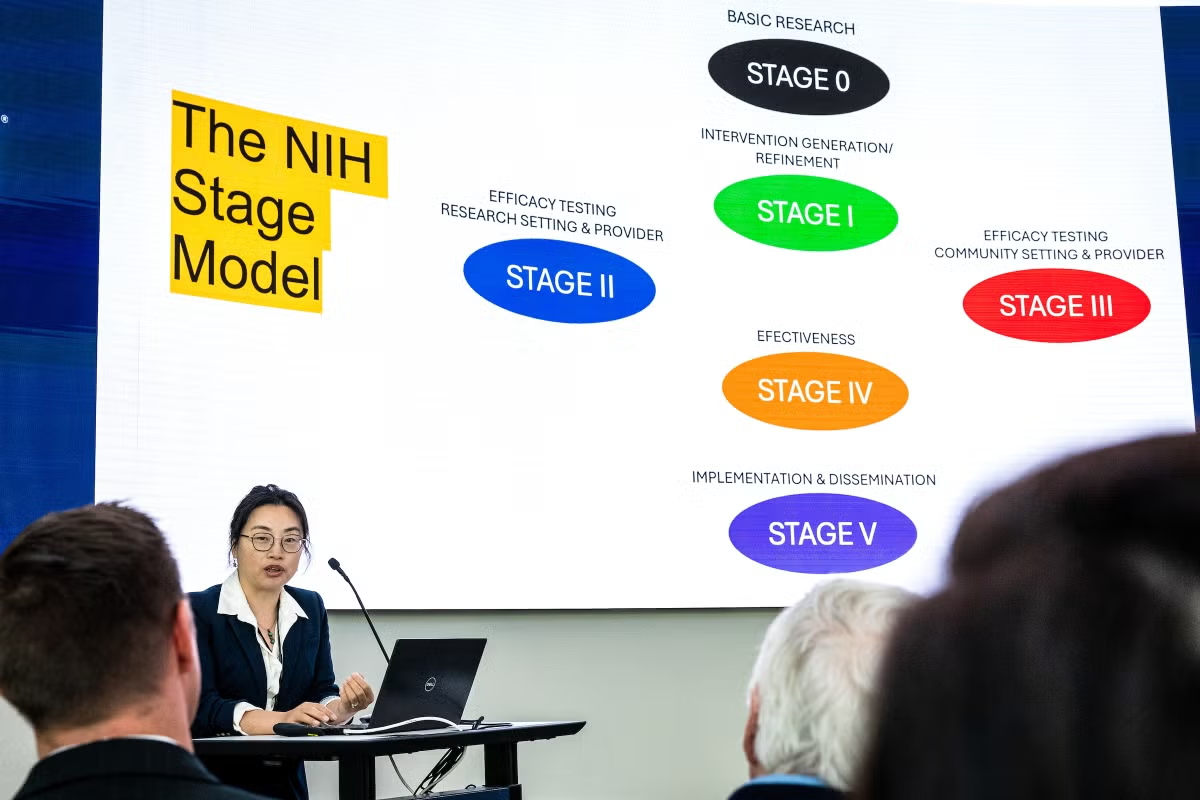
Lifestyle interventions, such as food and physical activity, are extremely effective in preventing Matthew BumanProfessor at the College of Health Solutions and Director of Precision Health Research Initiatives at College. But these interventions require many resources, such as several visits to several suppliers, and are difficult to implement on a large scale.
Digital health technologies can help.
“In fact, the elderly demand technology to support their health,” he said.
Buman participated in an opening address with Fang YuProfessor and President of EDSON in Translational Nurses of Dementia at Edson College of Nursing and Health Innovation.
They have described several studies in which digital devices help the elderly and their health care teams. In a study, the objective was to reduce the time that the elderly spent sitting and looking at screens, and how a combination of smartphones interventions, such as obtaining text alerts, winning them rewards and locking them up with their screens for a set of period, reduces the screen time by one hour a day.
“Digital twins” for interventions
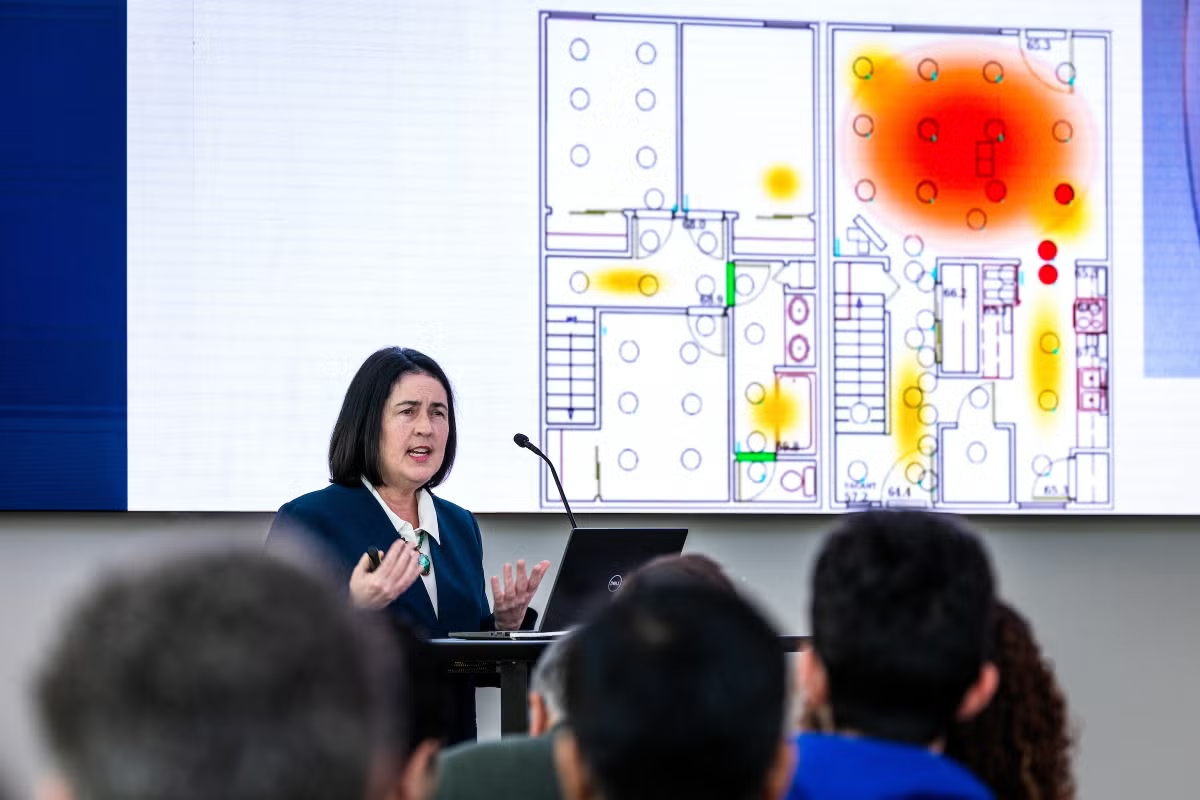
A “digital twin” is a virtual representation of a person based on data that helps predict how they will react to an intervention, according to the main speaker Diane Cook, professor at the School of Electrical Engineering and Computer Science at the Washington State University .
For example, a patient can suffer from type 2 diabetes but also cognitive decline.
“Let’s see his behavior, not only to detect the correlation between behavior and changes in his physical and cognitive health, but we can therefore see if there are controllable behaviors that could improve his health,” she said.
The digital twin will include data on genetics, social interactions and the environment.
Cook described the challenges of this method. Its laboratory has collected data on Apple watches and ambient sensors such as motion detectors, microphones and cameras in people’s houses. All this can measure if the person leaves the house and how active he is inside, but he cannot measure the functions such as the way in which he manages finances. In addition, the subject could remove the watch, make several activities both or live with several other people and pets.
But there is also a promise. For example, if a patient should take medication at dinner time, the model may see that the person is on the point of dinner but has not taken medication and that the patient may be invited.
Create human -centered technology
The summit included several sessions in small groups in addition to Keynotes. A panel addressed “Bridging the Digital Fivid: Ethics and Health Equity”.
Maissa KhatibA research scholarship holder of the College of Health Solutions, described how the Health design and innovation studio Created the cohort model of the Arizona community, a framework to establish confidence with a community.
“The entire premise is to have a community commitment at the start of a study, to identify the problems and to bring the members of the community to the possession of the project,” she said.
She said access to technology such as laptops and broadband internet connection cannot be held for certain populations.
Krystal TsosieDeputy professor at the School of Life Sciences, spoke of the native Biodata consortium in southern Dakota, the first non-profit research institute led by indigenous geneticists and tribal members in the United States
Tribal communities are wary of granting ownership of their data to other entities, Tsosie said. “The potential stigma of these genetic data is very real for them.”
She described how “group consent” is critical when working with tribal communities, as opposed to the Western concept of individual consent.
“It did not translate well in the way we structure our data models,” she said.
“It will be companies that benefit from free access models. They can benefit and hide behind an intimacy business veil. »»
Beza MeridDeputy Professor at the School for the future of innovation in the company, is director of the Laboratory of Digital Health and Racial Justice of the School. He said technology should not be considered a miracle solution.
“It is important to recognize that these technologies do not exist in a vacuum. They are designed by people who may have biases, who may have designed on the basis of executives that can be limited, “he said.
Merid said that blood pressure monitoring has gone from classic cuffs to wrist monitors and other more comfortable technologies. But now the work is done to design camera sensors that can measure blood flow towards the face.
“As used in racialized communities, facial recognition is inaccurate and is poorly used and mistreated,” he said.
Merger of innovation and health care
The medical field should be faster to adopt progress in digital health, according to Craig Norquist, an emergency doctor and information director with Honorhealth, the Main clinical affiliate For the new ASU medical school and advanced medical engineering.
Norquist, an ultramarathoner, described how athletes’ watches have evolved to measure oxygen levels and even sleep habits, but this technology was slow to adopt in medicine.
“We hesitated to try to implement new things. And there are reasons-we don’t want to try our luck on our patient, “he said.
“But I think we could probably do a little more than us.”
He described how the continuous glucose instructor was revolutionary for people with diabetes, who no longer had to stick their fingers before each meal.
“And when you incorporate this into the insulin pump, you essentially got a synthetic pancreas,” he said.
But the FDA refused to consider any technology that connected the two devices, considering it too risky. Revolutionary innovation occurred only because the patients themselves hacked the devices to have it communicated and then largely shared the information, said Norquist.
The pandemic has highlighted a lot of digital innovation, such as telemedicine, he said.
A team from the University of California in San Diego, used artificial intelligence to read chest x -rays to determine if the patients had a covid before there was a test.
“It therefore forced us to apply these tools for something other than something that will be put in a newspaper,” he said.
The partnership between Honorhealth and Asu is a way to infuse innovation in health care, he said.
“Continue to iterate, improve it, make it intuitive and make it work,” he said.